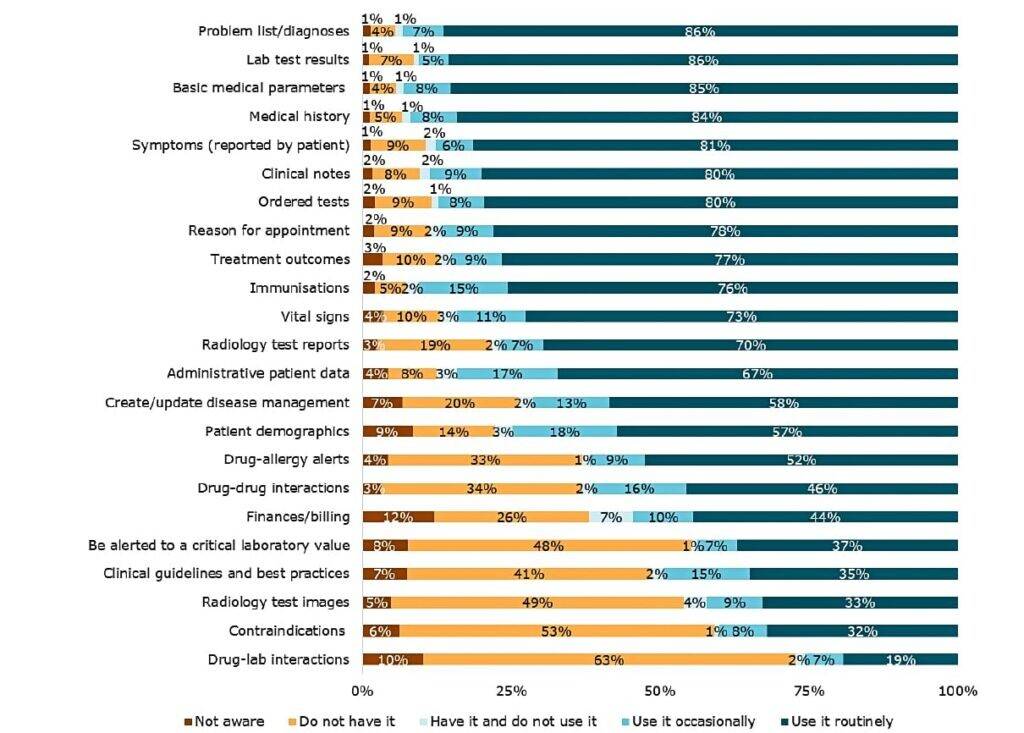
Countries with the highest level of adoption (Denmark, Estonia, Finland, Spain, Sweden and the United Kingdom) show that the use of eHealth is routine among GPs, while countries with the lowest level of adoption (Greece, Lithuania, Luxembourg, Malta, Romania and Slovakia) show that eHealth is currently not widespread. More than 80% of all GPs surveyed routinely use e-health functionalities like problem list/diagnoses (86%), lab test results (86%), basic medical parameters (85%), medical history (84%), symptoms (81%), clinical notes (80%), ordered tests (80%).
The study analysed different eHealth categories:
- Electronic Health Record (EHR) is currently available across all analysed EU countries, and nearly all GPs (96%) use it in their practice. Primary health data and information and order-entry functionalities are almost entirely adopted in all countries, and in more than half of the countries most GPs are routinely using clinical decision support functionalities and administrative data routinely.
- Health Informatics Exchange adoption is lower than EHR adoption. The degree of exchange of clinical, administrative and management is still not very high across the analysed countries. However, since 2013 there has been a substantial increase in the adoption of certifying sick leaves and transferring prescriptions to pharmacists; these are the functionalities with the highest increase.
- Telehealth shows progress, but its availability and use are still low in most analysed countries. Training and education functionalities are now available to half of GPs in the analysed countries, while they were only available to 36% of GPs surveyed in 2013. The availability of consultations with patients (12%) and telemonitoring (4%) is still low.
- Personal Health Record (PHR) adoption shows a similar pattern to Telehealth. The availability of the functionalities to request appointments and prescriptions has increased as well as the functionalities that patients can view their medical records and test results. However, there are some countries (Denmark, Estonia, Finland, Sweden and the United Kingdom) where these functionalities are more often available than in the other countries.
What influences the use of eHealth?
Among the factors that influence the use of eHealth are:
- Design and availability of applications;
- Motivations, attitudes and intentions;
- Perceived benefits, barriers and impacts;
- Institutional settings;
- Organisational settings;
- Community demands;
- Individual characteristics, social influence and networks.
The analysis of the drivers and barriers reported by the GPs showed that the practice settings are correlated with adoption levels.
On average, eHealth adoption is higher among countries with NHS system as compared to social insurance and transition countries. Denmark, Finland and Sweden are the countries with the highest scores among NHS countries; Ireland, Belgium and France have the most top scores among social insurance countries; and Estonia, Croatia and Czechia are leading among the transition countries. Overall, transition countries have lower levels of adoption compared to NHS and social insurance countries, with the exception of Estonia: it is not only ranked among the top five countries across all four eHealth categories and in the overall adoption of eHealth, but it also had the highest increase in the level of adoption since 2013.
34% of GPs think that eHealth has a positive impact on the doctor-patient relationship
In addition to the health system type, the type of practice is also associated with overall eHealth adoption. GPs working in health centres and group practices have higher adoption levels than those working in solo practices or under other arrangements (i.e. free-lance and others).
The variation in eHealth adoption is shaped by contextual meso- and macro-level factors, not only by GPs’ individual characteristics and attitudes. These results are similar to the 2013 study.
What do General Practitioners have to say?
The analysis of individual factors identified results similar to those in 2013. The majority of General Practitioners (GPs) surveyed consider ICTs to be useful for their practice, and think that their use increases the effectiveness of their practice and the quality of care. However, they are more sceptical about the impact on shorter waiting lists, patient satisfaction and the efficiency of consultations.
GPs also reported that ICT systems are easy to use and that they have the necessary technical assistance and resources to use them as well as the necessary knowledge to do so. However, in practice, they may not be able to decide whether or not to use a specific ICT functionality (this may depend, for example, on decisions taken by the public authorities or the managers of the health organisation). Social influences and peers are perceived as drivers of eHealth adoption. However, GPs also claimed a lack of positive eHealth impact on the doctor-patient relationship. Furthermore, financial difficulties, inter-operability issues, and lack of a legal framework on confidentiality and privacy are seen as the main barriers to eHealth adoption.
Perceived impacts and barriers were used to identify attitudinal profiles of GPs. The cluster analysis showed that:
- Realists are the largest group among the GPs. They consider both the obstacles and impacts as relevant and essential when it concerns the adoption of eHealth functionalities.
- Enthusiasts, representing the second large cluster in the sample, extol the impacts and disregard barriers.
- Indifferent GPs tend not to care about either impacts or barriers.
- Reluctant GPs place more importance on barriers than on impacts.
Compared to the 2013 results, there is a 10% decrease in the “Indifferent” group, while the “Enthusiast” group has increased from 13% to 27% between 2013 and 2018. This suggests that a large proportion of the GPs became more positive about the drivers and less negative about the barriers in the last five years.
Source: European Commission





