Besides, you would like to recruit active ambassadors that will proudly represent your service? Brilliant idea. You’d like to think of yourself as bold, not hesitating to take on new challenges and new ways of working together? Say no more. You have come to the right place. But wait a minute: before kick-starting the design thinking process to create the next game-changing service in healthcare, let us look at current standard business practices.
Good from far, but far from good
Although many of us are driven by the same motivations and ideas, striving towards the goal to make life easier for others, it seems that a big range of projects gets off on the wrong foot, resulting in services that are created without ever being used. Let’s have a look at the widely-spread business practices; It seems that a common approach is to assume what the problem and the solution is. So often, projects are being started with high ambitions, and let’s be honest, also a bit of a “know-it-all” attitude. Sounds a bit presumptuous?
To solve a problem by creating a novel service is especially problematic within the healthcare sphere. A patient organization or healthcare professional might not be open towards showing support for your service if they had no chance to be part of designing or building it. No matter how much of your heart you have poured into this, it is most often the notorious “not invented here” syndrome that makes healthcare professionals hesitant to represent your idea. And who can blame them for not wanting to advertise for a service they haven’t had any say in the making?
Co-creation is about involving end-users and relevant stakeholders
Long story short, we have been asked countless times “how on earth did you get that Key Opinion Leader (KOL) onboard to be an ambassador for your service?”, making us realize how big of an issue this is for both patient organizations and pharmaceutical companies. If we take an example of mobile apps, we can see many health apps are built with good intention.
However, the result of a somewhat assumptive approach to the real-life problems of the end-users, and not inviting them into the development process of the project, is something we often see ending on “the graveyard of apps.” The graveyard of apps, peacefully resting somewhere in cyberspace. When looking for health-related mobile apps, we find ourselves lost in an almost overwhelming amount of services. While the idea behind each one of them is in many cases very promising, only very few apps become well-implemented in daily-life routines of patients and healthcare professionals (HCPs).
To collaborate or to co-create, that is the question
What are our options to resolve these issues? Let’s look at different approaches to a project, going from your project being “closed” to being “open.” Thereby, we will think of a private corporation, for example, a pharmaceutical company as the product owner, and consider external stakeholders/end-users to be patients and HCPs.
1. Top-down, closed
In this approach, the product owner decides on the process, methods, content, and functionality. The product owner is relying on his or her knowledge and retain full control over the process. The available information about the end user's needs to build the service from is somewhat limited, so is the involvement of patients and HCPs.
2. Limited listening
Here, conversations are starting to be more open and receptive to input. Patients and HCPs may be asked in the beginning what their problems are. After this, there is no further external involvement in the project. Alternatively, the product owner might start building service and ask for external feedback along the way or in the end. Nevertheless, it is still the product owner who makes the decisions on what to take into consideration, what should be ignored, how the final product or service is going to look like, and how to get there.
3. Limited flexibility
A limited flexibility approach entails that the patients and HCPs can design some aspects of the solution, making the relationship more intimate. Patients and HCPs now get a specific set of responsibilities. For example, patients and HCPs might have been entitled to be in charge of one particular feature of the service. Nonetheless, the overall process and all other decisions remain fully controlled by the product owner.
4. Partnership
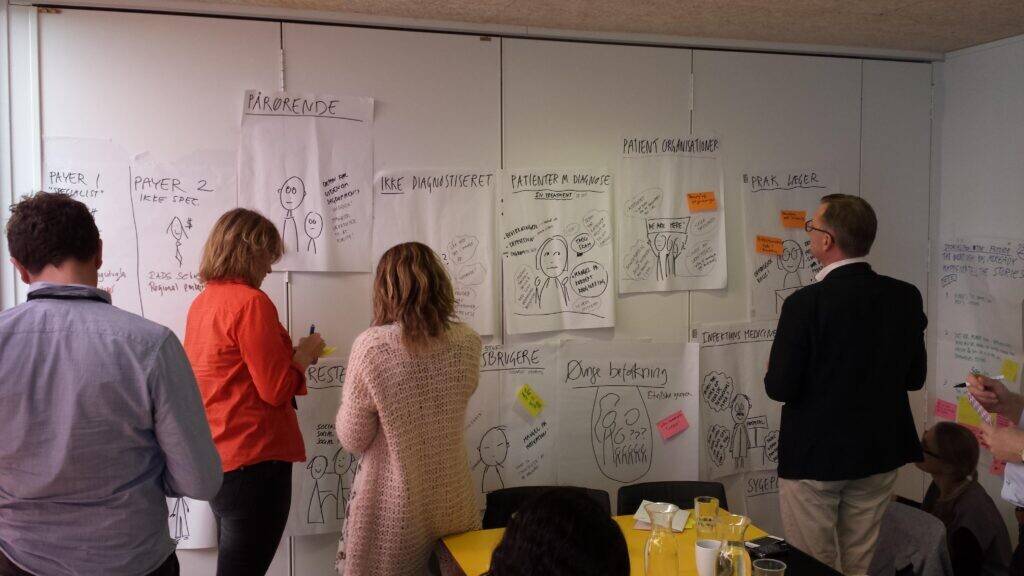
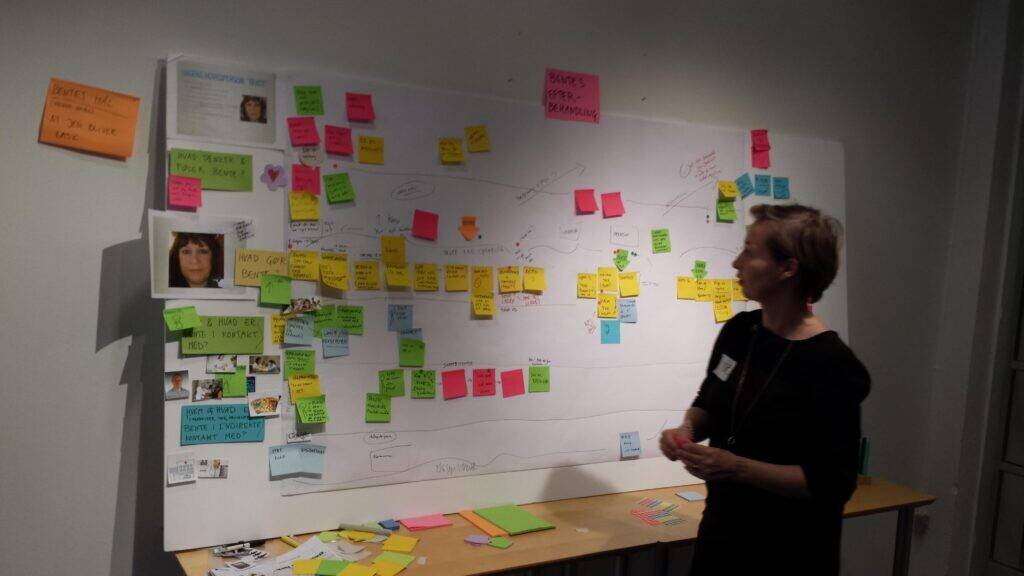
In a partnership, the entire process is co-owned and co-developed. The engagement of patients and HCPs is flexible and open, and a range of skills and different sets of expertise is included in the development, ensuring that the service fits the end-users needs and context. Decisions are then based on consensus and mutuality between the project sponsor, patients, and HCPs. If a service feature does not live up to everyone’s expectation, the design, functionality, or content of the feature will be revisited. It is the exact approach we define as co-creation: to be entirely inclusive towards patients and HCPs, to get all their minds and great ideas in one room, and to let them co-design.
“Co-creation is about involving end-users and relevant stakeholders to ensure that we create game-changing tools that meet actual daily-life requirements of patients and healthcare professionals,” says Lise Bové, Creative Strategist, Daman.
Essentials for successfully implementing new services in healthcare
The opportunity to innovate in healthcare is enormous, with several unique approaches and technologies being available. The rate of success is highly dependent on the four most important criteria with co-creation:
- Strong facilitation and leadership skills
- The right people
- An open mindset
- Rules






