In my previous article, we looked at the urgent need for the healthcare system to get back on its feet to face a perfect storm of postponed treatments, seasonal flu and a second wave of COVID-19. In this article, I’d like to discuss how new (and often involuntary) ways of working could play a hugely significant role in dealing with the curves I expect to follow this first phase of coronavirus. Because although we are living in an age of unprecedented challenge, we are also on the cusp of an extraordinary opportunity to restart the way we deliver healthcare.
With people working from home and all but the most essential travel discouraged, we have seen the widespread adoption of digital tools such as video conferencing – and healthcare has been no different. For many, this has been a reluctant shift imposed by circumstances. Yet in many cases, the transition is quickly overcoming initial resistance.
“Sectors that may normally be resistant to change, healthcare included, are now having change forced upon them and suddenly they realize hey! This actually works pretty well”
Video conferencing is highly applicable to numerous situations that do not need physical contact. Healthcare professionals forced to work at home due to COVID symptoms are now able to remotely assist their colleagues. Obstetricians are conducting most prenatal check-ins with virtual visits. Dermatologists are diagnosing less serious skin conditions via smartphones. And why expect a patient to visit the hospital to discuss an operation with the anaesthetist when a virtual meeting will work just as well?
On a wider scale, video is also facilitating contact between physicians, scientists and institutions around the globe through regular webinars – an essential part of the fight against COVID-19. And it is also the obvious way to safely stay in contact (or non-contact) with patients.
It’s efficient and it’s effective and it could be crucial too. Video meetings and telemedicine are cost-efficient, easy to fit into patients’ lives, free up physical space for complex conditions, and also support after-hours care.
Yes, necessity is driving digital healthcare and forcing large scale change in the smallest of timeframes. And yet… now the door has opened, just imagine what lies behind it. The same principle applies when it comes to monitoring patients in ICU. Digital tools such as a device on the wrist or a smart patch on the chest remotely monitor a number of vital signs, such as respiration, temperature, and pulse. This greatly reduces the number of standard checks-ups, allowing healthcare professionals to concentrate on those requiring acute care. Radboud University Medical Center, amongst others, have been the first one paving the way for years. Beyond streamlining the ways in which a unit works, this is also ideal for cases where patients need to be treated in other wards as ICU capacity fills up.
From temporary healthcare checks to permanent health monitoring
The next logical step is to take remote monitoring out of the hospital altogether. Smart patches can actually be more effective than incidental regular check-ups by a healthcare provider. The system immediately sends an alarm if the patient’s condition worsens, sometimes even before the patient or doctor is aware of this. The team can then chat with the patient via the secure platform about tweaking medication or setting new goals.
This kind of remote monitoring allows patients to remain at home for as long as possible before going to the hospital, then return earlier to recuperate in comfort. Patients treated at home tend to recover more quickly and require fewer tests and readmissions, all at less cost than a hospital. This also serves to alleviate the pressure on hospitals, freeing up beds for those who really need them such as today’s COVID-19 patients.
“Technology provides an unprecedented opportunity to deploy out of hospital. By remotely monitoring heart rate, respiration and temperature we can discharge many patients earlier and free up capacity sooner”
Remote monitoring paves the way to permanent monitoring based not on disease or treatment but on health in general. Look at the Apple Watch, one of the first medical-grade devices to sell over the counter without a prescription. Able to detect irregularity in the heart rate, it can send an ECG-style signal which the wearer can then share their doctor. And so we start to envision a seamless chain of integrated healthcare linking ICU to the general ward to the home. And in doing so, the transition from healthcare monitoring to health monitoring is complete.
Digital can help healthcare adapt to the way people now live their lives
With the advent of COVID-19, digital has now become an essential form of communication between hospitals and patients. Social media may be taken for granted in our personal lives, but this is far from being the case in healthcare where communication takes place by post and, believe it or not, even by fax at times. Again, coronavirus is changing that, brushing aside resistance at a stroke.
Social media is proving an ideal platform for sharing generic information with patients and families. Answers about repeat prescriptions and routine treatment can take place on community platforms. Advice for those feeling anxious staying at home. Proactive tips and tricks for diabetics. Now, the doctor’s surgery and the hospital ward come to the home. Digital is beginning to consign inefficient, paper-based communications to the waste bin where they belong.
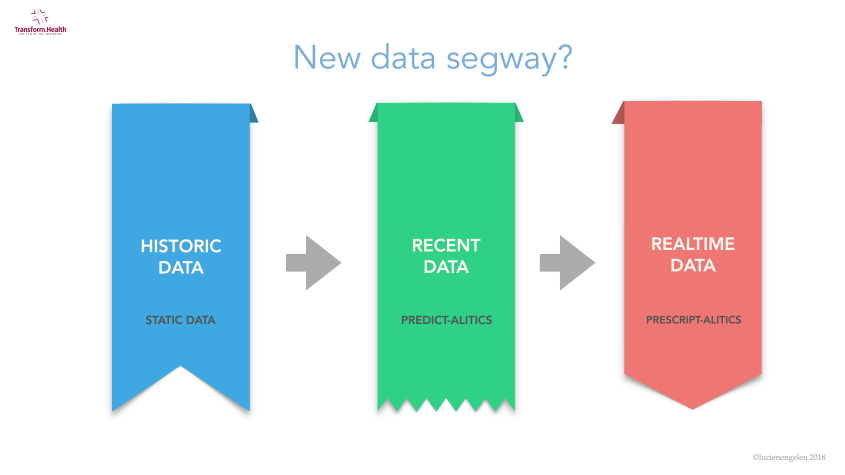
Up to now, healthcare procedures and protocols have been driven by historic data. That too is changing. Not only is recent data available (e.g. a patient’s MRI results from the same morning) but real-time data too. And while historic and recent information helps to inform a prediction, real-time data allows an instant prescription – and so we shift from reactive to proactive decision-making.
It’s time to put our priorities in order
Over the course of the last few weeks, we have also seen a reduction in the use of ineffective or low-value interventions such as medication, lab tests, prenatal interventions, and diagnostic/surgical procedures. Now the focus has shifted to the preservation of capacity and invaluable supplies of PPE, hospitals have postponed and canceled myriad elective procedures from steroid injections to spinal screws to PET scans. Patients are no longer being admitted for tests to rule out rare conditions.
Has COVID-19 provided the unexpected opportunity to cut out this slack from the system? If physical therapy is a more effective treatment for arthritic knees than expensive steroid injections, isn’t the choice than obvious?
Same thing for using medication to treat stable, moderate-to-severe chest pains as opposed to costly procedures like catheterization and stent placements, or prescribing physical and behaviour therapy for back pain rather than spinal injections and surgery. This is our chance to look at the procedures that have been postponed without creating issues and ask: are they needed after all?
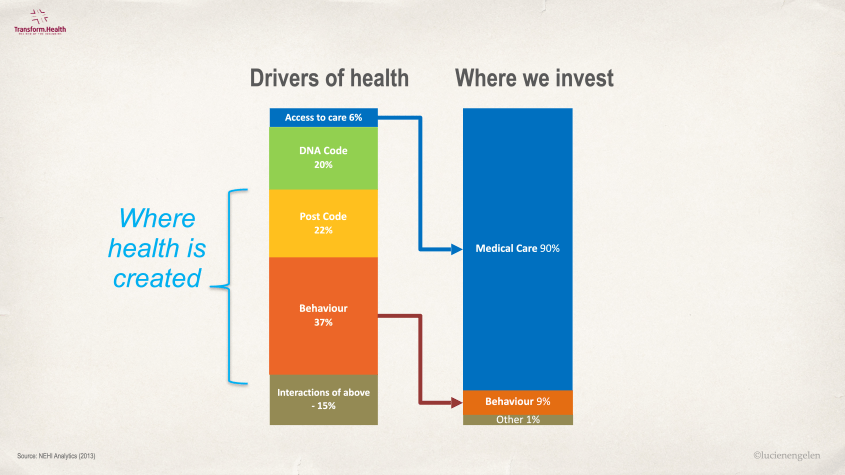
Reassess the way we invest in the provision of health care
What determines health? As we know, a combination of genetics and birthplace are the major influencers. By contrast, the local healthcare system determines just six percent of one’s health – and yet it accounts for 90 percent of healthcare expenditure. When you think about it, these numbers are so disproportionate it’s crazy. Why not target this investment to the front end? I’m not just talking about prevention here, but a value-based, personalized approach to health. Surely that makes more sense than continuing to do things ‘just like we always have’ because, well, that’s what we always do.
This could open up truly exciting opportunities across a number of fronts, linking our ongoing health to other aspects of life
For example, why not use food and nutrition data to make beneficial foods cheaper than non-beneficial ones depending on any individual’s needs?
Take patients undergoing chemotherapy. They will receive a good level of care in the hospital and all the right foods, but after that, they are pretty much on their own. Yet it’s so easy to ensure guidance on the correct nutrition continues after they return home.
Or we could link healthcare to finance. We know that people in financial debt are more likely to use the healthcare system. But what if banks offered to spread the debt and lower the interest, a cost underwritten by healthcare insurers who in doing so reduce their own costs? Suddenly, all the edges between healthcare and nutrition, finance, technology, etc. interconnect to provide a robust, personalized, preventative healthcare system.
Digital-first, physical next. This is our opportunity to unlock a better way of working
The digital genie is well and truly out of the bottle. So, I ask: why should we ever go back to the way we’ve always done things? We know large scale emergencies are set to occur over and over again, whether earthquakes, fires or pandemics. Digital prepares us for these challenges, allowing us to take as much burden off the system as we can. Because over the next two decades, there is no way today’s healthcare systems are going to cope with growing demands.
We face a lack of skills, huge burnout rates, and people leaving the sector earlier than they should because they can no longer cope. At the same time, not enough replacements are entering the system, scared off by the idea of being undervalued and overworked. The back door is wide open while the front door almost closed. Yet the way to stay on control is right in front of our eyes.
And when you think that healthcare is 80 percent blunt logistics from a patient perspective – talking to a doctor, fetching a prescription, etc., and only 20 percent is actually medical, just imagine to what extent digital can shift the focus back to nursing and treatment, allowing doctors and nurses and specialists to do what they actually signed up to do.
COVID-19 has shown that even more patients can be treated well without being hospitalized. Digital technologies alongside intelligent automation, product innovation can build on this to utterly transform the way we work
Reimagine the future
Reimagine the future cannot come a day too soon… I believe that the ideas, insights, and innovations we capture now can help us to reset the future of healthcare delivery. As Why becomes why didn’t we do this before? we are faced with the unprecedented opportunity to step back and look at which parts of the process really do add value and which do not, and how processes can be organized to minimize time and effort by making the most of video conferencing, remote monitoring, data analysis and communicating information in a language understandable to everyone.
Technology can help keep healthcare effective, safe, resilient, accessible and affordable. It can provide healthcare institutions with the freedom to function as optimally as possible for everyone. We are not there yet, and truth be told we’re not even close. But let’s not miss this one-off opportunity to secure the future. Now is the time to reimagine our approach. Now is the time to reset our expectations. Now is the time to restart healthcare.