Healthcare managers are increasingly aware of the impact of digitization on process efficiency, patient service quality, and employee satisfaction. They choose systems thoughtfully, carefully calculating their fit with the other elements of the digital ecosystem and clinical workloads. They are not just purchasing IT systems anymore but investing in reasonable solutions, expecting the highest quality implementation and well-calculated return on investments. This new approach to digital transformation comes from a growing understanding of the role of digital health solutions.
Digitally orchestrated patient journey
Digitalization is too essential to be a matter of uncoordinated and random decisions. Thus, hospitals establish dedicated innovation departments to navigate e-health and select innovative solutions with added value to support facility operations and its competitive edge. IT investments are integrated into strategies and development plans to create a consistent patient journey that meets the needs of staff and patients while also building a unified database ready to implement AI solutions. Individual priorities may vary, but the priority is maximizing patient outcomes while minimizing administrative burden.
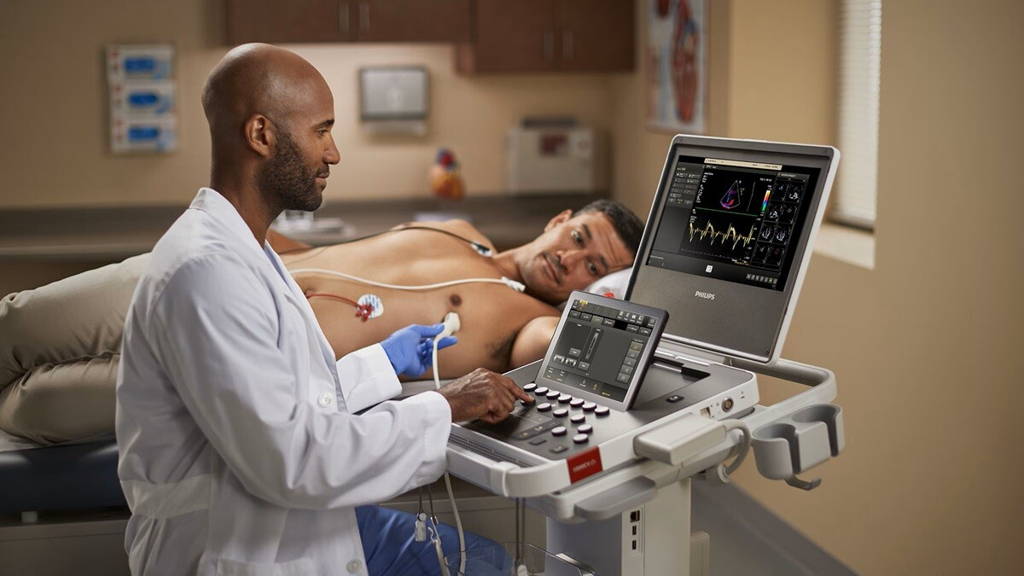
Digitization is intended to work smoothly in the background, supporting healthcare professionals and enabling workflow streamlining.
A continuous process interwoven into organizational development
Digital transformation is an endless process requiring updates, introducing previously unused functionalities, staff retraining, assessing new tools and gaining competencies like data engineering. A strong relationship with the IT system provider is crucial to manage this process effectively. The IT company's service team knows the system from the outside down and its functionalities; they can advise on reconfiguring systems for easier use and suggest best use cases observed in similar settings. They can also manage change associated with digitization, engage employees, communicate the following steps, sustain motivation by demonstrating benefits, and address skepticism about innovation.
Some managers implement management by objectives, allocating a budget in each organizational unit for digitalization and treating e-health solutions as investments rather than costs. This approach allows for measurable and valuable effects. Savings on IT in the long run lead to poor patient satisfaction and staff frustration. It can be dangerous in terms of increased vulnerability to cyber risks.
HB-HTA for the most advanced innovators
At the highest level of innovation maturity is the Hospital-Based Health Technology Assessment (HB-HTA) methodology. It's a process for assessing the rationale, benefits, and effects of implementing health technologies and interventions to help hospital managers make more informed investment choices. However, it requires considerable organizational effort, including dedicated teams of physicians, finance staff, and IT specialists.
Variables to be evaluated are safety of use, cost, strategy compliance, cost-effectiveness, treatment quality, convenience impact, etc. HB-HTA involves developing qualitative and quantitative measurement indicators, systematically collecting evidence on technology, simulating its impact post-implementation, and assessing cost-effectiveness, as well as implications for existing procedures.
Implemented but not evaluated: telecare
Still, only a marginal percentage of healthcare facilities are measuring the quality of telehealth, which was rapidly implemented during the COVID-19 pandemic. They are frequently used as a 1:1 replacement for on-site visits, even if some studies suggest telecare is not always the best way of healthcare delivery. And vice-versa: some medical services are still delivered only in healthcare facilities when they could be more accessible online while at the same quality. Outcomes are rarely monitored, and only a few countries have clear telemedicine guidelines.
WHO Regional Office for Europe recently launched a Telehealth quality of care tool, including a self-assessment tool and various frameworks, that can assist facilities in improving telehealth services and ensuring safe, equitable, patient-centered care. It is aligned with the ISO 13131:2021 standard. Thus, it can serve as both a guidance and self-assessment instrument for quality improvement telehealth services at local, regional, and national levels.
Current reimbursement models in most healthcare systems have not promoted the quality of medical services. However, that is beginning to change thanks to greater accessibility to data collected in the health system. Utilizing approaches to assess the value of IT solutions allows for strategic digital growth, addressing specific bottlenecks in patient care rather than chasing cutting-edge innovations.