What are your biggest hopes regarding digital health?
This is a tough question because high hopes for digital health or eHealth have been expressed for so many years by so many people. My hope is that digital health can be used to act on priorities like reducing medical error and fraud, providing equal access to quality care, and facilitating the patient-physician relationship.
Unfortunately, at the same time, not all about digital is positive. Digital systems can introduce errors. Hackers target health data. Many doctors spend more time on electronic medical records than on communicating with the patient. Silicon Valley is no longer as highly regarded, etc.
Which issues of technological transformation should be discussed more often?
Here are some of the main ones.
- The time required to do clinical trials and satisfy regulatory requirements versus the life cycle of the technology;
- The excess of choice that comes from too many innovations, both complicating interoperability and wasting resources;
- The non-alignment of incentives amongst the different stakeholders which slows down the distribution of innovation;
- Our difficulty in developing a truly new vision for healthcare. If I take an example from consumer products, a well-funded startup called Quibi has a new vision for culture: that while cinema and tv have each generated their media (films and tv shows), smartphones have not. So they’re developing a new medium for smartphones, the short-form video that can be watched vertically and horizontally. Entertainment is not as complex or critical to us as healthcare, but it’s interesting to note that this company proposes a new vision.
What is "ethical digital innovation” in healthcare?
Ethical digital innovation is, so far, a dream goal, as is truly ethical healthcare. But we are trying hard to achieve that. Such an innovation would be:
- conceived for the benefit of the patient,
- accessible to all patients,
- fully personalized,
- based on representative data,
- carbon-neutral.
And let’s add the five principles cited in a Nature publication and which are embedded in my first criterion “for the benefit of the patient”: transparency, justice and fairness, non-maleficence, responsibility, and privacy.
What's your opinion about the market of wearables today?
The wearables market is growing and currently led by devices that track fitness and wellbeing, such as watches, which account for around half the market. Google purchased Fitbit in November 2019, after previously purchasing Fossil for its smartwatch technology. Google’s actions are a solid, short-term sign of potential, although Google can withdraw in the future as easily as it entered. Sleep tracking is also growing. Both fitness and sleep are essential to preventive health.

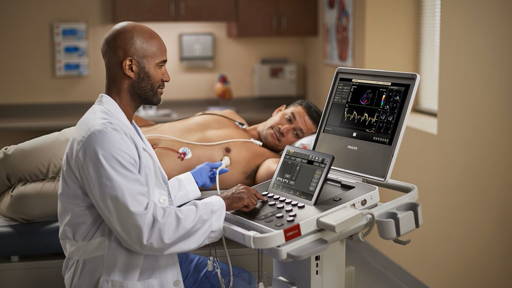
On the medical side, interest in the EKG-related applications of connected objects has matured, although the value of the identification of largescale, symptomless cardiac irregularities has not been demonstrated. Cardiology lends itself particularly to tracking, and there are so many medical segments with connected objects that we can’t mention them all here! Such listings are the bread and butter of the companies that sell market research reports!
Could you please name one innovation that interested you recently?
I was excited to see Medwand receive various awards at CES 2020. Medwand, which was developed by a physician, is like a StarTrek tricorder but with seven tools that fit in your palm and enables a physician to “examine” a patient anywhere in the world. Medwand includes a stethoscope, otoscope, ophthalmoscope, dermatoscope, thermometer, it does an EKG, measures blood oxygen levels.
Medwand has been in development for at least five years, but the buzz it got at CES has come at the right time, in that teleconsultation financed both by insurance plans and by the consumer has risen considerably. In medical deserts, we can imagine a municipality owning several of these and renting or lending them out to families. In a city, there could be one or several per building and, of course, in pharmacies, etc. The price was positioned at $399.
Digital health needs to be embedded in the conception of the health system
Your experience in digital health spans more than 20 years. Let's go back in time to the year 2000. How did you imagine healthcare in 2020?
I imagined then that by 2020, we would live in a world of medical co-decision, shared by professionals and patients, with useful information at the disposal of all, thanks to online publication and communities, with a universal electronic medical record for each user, and that telemedicine would be very widely available, enabling each patient to be matched to the most appropriate professionals, a personalized care team, anywhere in the world.
In 2003, upon the occasion of the European Commission’s first high-level conference on eHealth, I was asked by the EC to produce a report on “the Case for eHealth.” I wrote in that report that “e-Health is the single-most-important revolution in healthcare since the advent of modern medicine or hygiene.” The report was very well-received and has been cited over 100 times in peer-reviewed articles around the world.
I still think that eHealth or digital health has that high potential, but given all the limitations that slow down its distribution, digital health needs to be embedded in the conception of the health system.
Are we transforming healthcare in the right way, or could we make some changes?
As concerns the transformation of healthcare for existing medical conditions, we need to involve patients as partners from A to Z. As you might have guessed, greater compassion heals more. If patients helped establish the priorities, healthcare would be organized differently, and professionals would be the first to benefit as well.
How do you imagine healthcare in 2030?
It will be different in 2030 than whatever I imagine now. Here are a few thoughts nonetheless:
- teleconsultation and device-supported teleconsultation will become widespread;
- trackers will have helped people increase the number of daily steps significantly;
- closed-loop diabetes systems will be used by the majority of patients with type 1 diabetes;
- therapeutic Virtual Reality will be widely offered for pain, anxiety, and rehabilitation;
- the quality of X-rays and EKG readings will have increased thanks to AI-supported clinicians;
- there will be better patient-physician communication and more co-decision making.
Denise Silber is a leading digital health strategist, communicator, and influencer. Denise created and leads Doctors 2.0 & You Events and Services, bringing digital health tools, start-ups and patient engagement sessions to events for physicians internationally. With her combined experience as a senior pharma executive and entrepreneur, Denise is a frequent master of ceremonies and keynote speaker to diverse healthcare audiences internationally and also advises start-ups. Denise was awarded the French Legion of Honor in 2011, for her contribution to eHealth, and recognized as one of the #InspiringFifty women in tech in France in 2018. The dual US and French citizen, Denise did her undergraduate degree in Government at Smith and was a US Foreign Service Officer, before receiving her MBA from Harvard. Based in Paris, Denise serves as vice-president of the Harvard Club of France.